Cardiac heart arrhythmias
|
What is cardiac arrhythmia? What types of cardiac arrhythmias are there? What causes cardiac arrhythmias? What're the symptoms of cardiac arrhythmia? How is cardiac arrhythmia diagnosed? What're the treatments for cardiac arrhythmia? What happens during an arrhythmia? What is a heart block? What are the symptoms of an arrhythmia? How is an arrhythmia diagnosed? How does the doctor know that I have arrhythmia How are arrhythmias treated? What happens in the heart during an arrhythmia? How can arrhythmias be prevented? Are arrhythmias serious? | ||||||||
|
What are shockable pulseless cardiac arrest rhythms? What are nonshockable pulseless cardiac arrest rhythms? When do you use epinephrine in a medical emergency? When do you use atropine in a medical emergency? What is the dose of epinephrine for pulseless cardiac arrest rhythms? What is the dose of atropine for pulseless cardiac arrest rhythms? | ||||||||
|
Cardiopulmonary resuscitation (CPR)
A combination of chest compressions and assisted breathing performed when the electrical and pumping function of a person's heart is not working. Typically performed when the heart in ventricular fibrillation or asystole. | ||||||||
|
CPR is divided into three support stages: * Basic life support * Advanced life support * Prolonged life support. | ||||||||
|
The first Advanced Cardiac Life Support class was taught at an AMA joint meeting with American Heart Association in 1978.
Designed primarily for physicians: 1) Cardiologists 2) Internal medicine specialists 3) Medical students 4) Emergency Medicine specialists | ||||||||
|
Overview * Anatomy and Physiology | ||||||||
| Rhythm Categories | ||||||||
Sinus Rhythms
| ||||||||
Atrial Rhythms
| ||||||||
Junctional Rhythms
| ||||||||
Ventricular Rhythms
| ||||||||
Heart Blocks
| ||||||||
Miscellaneous Rhythms
| ||||||||
|
The prognosis in asystole depends on the etiology of the asystolic rhythm, timing of interventions, and success or failure of advanced cardiac life support (ACLS).
SHOCKABLE RHYTHMS NONSHOCKABLE RHYTHMS Four rhythms produce pulseless cardiac arrest: ventricular fibrillation (VF), rapid ventricular tachycardia (VT), pulseless electrical activity (PEA), and asystole. Survival from these arrest rhythms requires both basic life support (BLS) and advanced cardiovascular life support (ACLS). Out of hospital cardiac arrest data have observed better outcomes for patients with PEA than asystole. | ||||||||
| What Is a Normal Heart Rhythm? | ||||||||
| What is Asystole? | ||||||||
| What are the causes of sudden cardiac arrest? | ||||||||
| What is fibrillation? | ||||||||
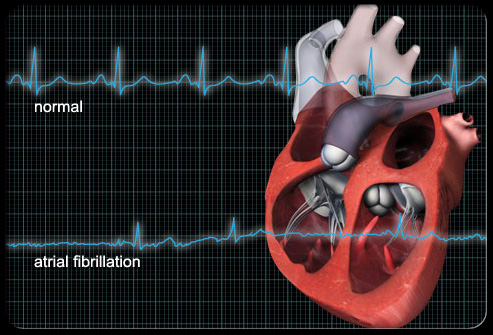
What is atrial fibrillation?
 | ||||||||
| ||||||||
|
What is ventricular fibrillation? What is cardioversion? What is a defibrillator? | ||||||||
|
Ventricular Tachycardia 1. What is ventricular tachycardia? 2. Is this a life-threatening arrhythmia? 3. What causes ventricular tachycardia? 4. What are the treatment options for ventricular tachycardia? 5. What is the success rate for the cardiac catheter ablation procedure for ventricular tachycardia? | ||||||||
| Your coronary arteries | ||||||||
| Coronary Artery Disease | ||||||||
|
ADVANCED CARDIOVASCULAR LIFE SUPPORT RHYTHM INTERPRETATION a. Airway management b. Arrythmias, Defibrillation, and Pacing c. IV Access, Resuscitation, Circulatin, and Monitoring d. Infant CPR and Ventilation e. Review Questions f. Appedices: Pharmacology, Algorithm Protocols g. Chamber Abnormalities and Intraventricular Conduction Defects h. SA and AV Nodal Block i. Ischemia and Infarction j. Reentrant Supraventricular Tachycardias k. Ectopic Supraventricular Tachycardias l. Extrasystoles and Pre-excitation Syndromes m. Differential Diagnosis of Wide QRS Tachycardias n. Medication and Electrolyte Effects, Miscellaneous Conditions o. Electronic Pacemakers 4-1: the monitor 4-2: the capacitor 4-3: the numbered buttons 1,2,3; output dials 4-4: the paddles and the pads 6-1: Cardioverting a-fib. 6-2: Cardioverting VT-with-a-pressure. How do I defibrillate someone? 7-1: Defibrillating VT 7-2: Defibrillating VF 8-1: Using synchronization correctly. 8-2: Keeping the process orderly. 8-3: Clearing the bed. 8-4: Using contact gel properly contact burns. What is fibrillation? What is atrial fibrillation? | ||||||||
| www.arrhythmia.org/ general/whatis/ | ||||||||
|
Supraventricular Tachycardia
1. What is supraventricular tachycardia? 2. Are there different types of supraventricular tachycardia? 3. What causes supraventricular tachycardia? 4. What are treatment options for this heart rhythm irregularity? 5. What is the success rate of the cardiac catheter ablation procedure when used for supraventricular tachycardias? | ||||||||
|
How do defibrillators work? What is depolarization? What does electricity have to do with it? What is a joule? What is monophasic defibrillation? What is biphasic defibrillation? What is Transthoracic Impedance? How do I cardiovert someone? What bad things do I have to watch for during cardioversion or defibrillation? What things should I do after the cardioversion/defibrillation? What is cardioversion? What is a defibrillator? How do defibrillators work? What is depolarization? What does electricity have to do with it? What is a joule? What is monophasic defibrillation? What is biphasic defibrillation? What is transthoracic impedance? How do I cardiovert someone? http://www.virtualcpr.com/images/defib_pos.jpg How do I defibrillate someone? What bad things do I have to watch for during cardioversion or defibrillation? What things should I do after cardioversion/defibrillation? What is cardioversion? Why is the cardioversion procedure needed? Where is the procedure performed? Should I take my medications? Can I eat before the procedure? What should I wear? What should I bring? What happens before the procedure? Will I be monitored? Will I be awake during the procedure? What happens during the procedure? How long does the procedure last? Will I have to stay in the hospital? What should I expect during the recovery? How will I feel after the procedure? What is an arrhythmia? How do I know if I have an arrhythmia? What are the treatment options? What medication is available for arrhythmias? What is cardioversion? What are the ablation options? What implantable devices are used to treat arrhythmias? What if I do nothing? Is catheter ablation a good choice? Why choose cryoablation? How do I prepare for cryoablation? What is the experience of cryoablation patients? What can I do next? | ||||||||
|
What is an arrhythmia? How common are arrhythmias? What are the clinical symptoms? What causes arrhythmias? What are the consequences of arrhythmias? How are arrhythmias treated? What is an arrhythmia? An arrhythmia (ah-RITH-me-ah) is a problem with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm. A heartbeat that is too fast is called tachycardia (TAK-ih-KAR-de-ah). A heartbeat that is too slow is called bradycardia (bray-de-KAR-de-ah). Most arrhythmias are harmless, but some can be serious or even life threatening. When the heart rate is too fast, too slow, or irregular, the heart may not be able to pump enough blood to the body. Lack of blood flow can damage the brain, heart, and other organs. The rhythm of the heart is normally generated and regulated by pacemaker cells within the sinoatrial (SA) node, which is located within the wall of the right atrium. SA nodal pacemaker activity normally governs the rhythm of the atria and ventricles. Normal rhythm is very regular, with minimal cyclical fluctuation. Furthermore, atrial contraction is always followed by ventricular contraction in the normal heart. When this rhythm becomes irregular, too fast (tachycardia) or too slow (bradycardia), or the frequency of the atrial and ventricular beats are different, this is called an arrhythmia. The term "dysrhythmia" is sometimes used and has a similar meaning. How common are arrhythmias? About 14 million people in the USA have arrhythmias (5% of the population). The most common disorders are atrial fibrillation and flutter. The incidence is highly related to age and the presence of underlying heart disease; the incidence approaches 30% following open heart surgery. What are the clinical symptoms? Patients may describe an arrhythmia as a palpitation or fluttering sensation in the chest. For some types of arrhythmias, a skipped beat might be sensed because the subsequent beat produces a more forceful contraction and a thumping sensation in the chest. A "racing" heart is another description. Proper diagnosis of arrhythmias requires an electrocardiogram, which is used to evaluate the electrical activity of the heart. Depending on the severity of the arrhythmia, patients may experience dyspnea (shortness of breath), syncope (fainting), fatigue, heart failure symptoms, chest pain or cardiac arrest. What causes arrhythmias? A frequent cause of arrhythmia is coronary artery disease because this condition results in myocardial ischemia or infarction. When cardiac cells lack oxygen, they become depolarized, which leads to altered impulse formation and/or altered impulse conduction. The former concerns changes in rhythm that are caused by changes in the automaticity (spontaneous activity) of pacemaker cells or by abnormal generation of action potentials at sites other than the SA node (termed ectopic foci). Altered impulse conduction is usually associated with complete or partial block of electrical conduction within the heart. Altered impulse conduction commonly results in reentry, which can lead to tachyarrhythmias. Changes in cardiac structure that accompany heart failure (e.g., dilated or hypertrophied cardiac chambers), can also precipitate arrhythmias. Finally, many different types of drugs (including antiarrhythmic drugs) as well as electrolyte disturbances (primarily K+ and Ca++) can precipitate arrhythmias. What are the consequences of arrhythmias? Arrhythmias can be either benign or more serious in nature depending on the hemodynamic consequence of the arrhythmia and the possibility of evolving into a lethal arrhythmia. Occasional premature ventricular complexes (PVCs), while annoying to a patient, are generally considered benign because they have little hemodynamic effect. Consequently, PVCs if not too frequent, are generally not treated. In contrast, ventricular tachycardia is a serious condition that can lead to heart failure, or evolve into ventricular fibrillation and cause death. How are arrhythmias treated? When arrhythmias require treatment, they are are treated with drugs that suppress the arrhythmia. These drugs are called antiarrhythmic drugs. There are many different types of antiarrhythmic drugs and many different mechanisms of action. Most of the drugs affect ion channels that are involved in the movement of sodium, calcium and potassium ions in and out of the cell. These drugs include mechanistic classes such as sodium-channel blockers, calcium-channel blockers and potassium-channel blockers. By altering the movement of these important ions, the electrical activity of the cardiac cells (both pacemaker and non-pacemaker cells) is altered, hopefully in a manner that suppresses arrhythmias. Other drugs affect autonomic influences on the the heart, which may be stimulating or aggravating arrhythmias. What happens during an arrhythmia? What is a heart block? What are the symptoms of an arrhythmia? How is an arrhythmia diagnosed? How does the doctor know that I have arrhythmia How are arrhythmias treated? What happens in the heart during an arrhythmia? How can arrhythmias be prevented? Are arrhythmias serious? What are the symptoms of an arrhythmia? Most people have felt their heart beat very fast, experienced a fluttering in their chest, or noticed that their heart skipped a beat. Almost everyone has also felt dizzy, faint, or out of breath or had chest pains at one time or another. Symptoms may include: * palpitations (increased awareness of the heart beating faster) This is often the only symptom for most people. * chest pain * shortness of breath * lightheadedness or fainting * fatigue or weakness You should not panic if you experience a few flutters or your heart races occasionally. But if you have questions about your heart rhythm or symptoms, check with your doctor. How does the doctor know that I have arrhythmia Arrhythmia's (also called dysrhythmias) may occur at any age. Sometimes a person may not be aware they have an arrhythmia. The usual ways to evaluate a rhythm abnormality are similar to those used to evaluate other health problems. The patient's history is very important. Questions like these might be asked: * Are you aware of unusual heartbeats? * Does anything bring on the arrhythmia? What can you do, if anything, to make it stop? * If it's a fast rate, how fast? * Do you feel weak, lightheaded or dizzy? * Have you ever fainted? Some medicines may make arrhythmias worse. It's important to tell the doctor about all prescribed and over-the-counter medicines that you take. What happens in the heart during an arrhythmia? An arrhythmia may occur for one of several reasons: * Instead of beginning in the sinus node, the heartbeat begins in another part of the heart. * The sinus node develops an abnormal rate or rhythm. * The signal bypasses the normal regulation of the AV node * A patient has a heart block. Are arrhythmias serious? Many arrhythmias occur in people who do not have underlying heart disease. The vast majority of people with arrhythmias have nothing to fear. They do not need extensive exams or special treatments for their condition. In some people, arrhythmias are associated with heart disease. In these cases, heart disease, not the arrhythmia, poses the greatest risk to the patient. In a very small number of people with serious symptoms, arrhythmias themselves are dangerous. These arrhythmias require medical treatment to keep the heartbeat regular. For example, a few people have a very slow (bradycardia) or fast (tachycardia) heartbeat. These patients may have symptoms such as chest pain, shortness of breath, lightheadedness or fainting because the heart is not pumping enough blood to the body. If left untreated, the heart may stop beating and these people could die. Devices: Pacemakers 1. What will a pacemaker do for me? A pacemaker will ensure that your heart rate will not beat too slowly because of its inability to deliver electrical impulses when needed. A minimum heart rate is programmed into the pacemaker by the physician so your pulse will not go below this rate. It is recommended for people who have slow heart rates accompanied by symptoms such as dizziness, lightheadedness or passing out. Some people have rapid heart rhythms that require medications to control symptoms by reducing the heart rate. In this case, implantation of a pacemaker might be needed to allow this treatment. 2. What are the restrictions after I have a pacemaker implanted? For the first two weeks after implantation of the pacemaker, the restrictions are as follows: * Do not lift the arm on the side that the pacemaker was implanted any higher than your shoulder. This will reduce the risk of dislodging the leads (wires) that were placed in your heart muscle and attached to your pacemaker. * No lifting of greater than 10 pounds. * Avoid sleeping on the same side that the pacemaker is implanted on while the wound is healing. For a total of eight weeks after implantation: * No vigorous swinging of the arm on the side that the pacemaker is implanted, such as would occur with activities like golf, tennis, baseball, etc. Some other things to be avoided after a pacemaker is implanted: * Magnetic resonance imaging (MRIs) * Contact with magnetic wands that are used in airports for personal search * High power magnetic or electrical fields 3. How often do I have to have the pacemaker replaced? Pacemakers are generally replaced every six-to-eight years. You will be scheduled for routine follow-up at the Pacemaker Clinic to check for normal functioning and remaining generator life to anticipate when it will need to be replaced. Devices: Cardioverter-defibrillators 1. What does a cardioverter-defibrillator do? An implantable cardioverter-defibrillator (ICD) is able to deliver a shock to the heart when dangerous, life-threatening arrhythmias occur. All ICDs are also able to provide cardiac pacing if needed for slow heart rates. ICDs can be recommended when someone has: * A severely weakened heart muscle * Evidence of life-threatening arrhythmias that produce symptoms and cannot be controlled with treatment * History of cardiac arrest 2. How do pacemakers and ICDs differ? Pacemakers can only make sure that your heart rate will not go too slow. ICDs can monitor for life-threatening arrhythmias and deliver a shock if necessary. Both types of devices can provide pacing if needed. 3. How often do I have to have the cardioverter-defibrillator replaced? ICDs are generally replaced every four-to-six years depending on how much it is used for pacing and how many shocks it delivers. You will be scheduled for routine follow-up at the ICD clinic to check for normal functioning and remaining generator life to anticipate when it will need to be replaced. 4. Are there any restrictions after I have the ICD implanted? For the first two weeks after implantation of the ICD, restrictions are as follows: * Do not lift the arm on the side that the ICD was implanted any higher than your shoulder. This will reduce the risk of dislodging the leads (wires) that were placed in your heart muscle and attached to your ICD. * No lifting of greater than 10 pounds. * Avoid sleeping on the same side that the ICD is implanted while the wound is healing. For a total of eight weeks after implantation: * No vigorous swinging of the arm on the side that the ICD is implanted, such as would occur with activities like golf, tennis, baseball, etc. Some other things to be avoided after an ICD is implanted are: * Magnetic resonance imaging (MRIs) * Contact with magnetic wands that are used in airports for personal search * High power magnetic or electrical fields * Arc welding | ||||||||
|
http://my.clevelandclinic.org/heart/services/tests/procedures/cversion.aspx http://www.texasheartinstitute.org/HIC/Anatomy/conduct.cfm http://equimedcorp.com/rhythms/topic/51/ http://www.learnekgs.com/learnecgrules.htm http://cal.vet.upenn.edu/projects/anestecg/Basics/smartrev.htm http://www.medicinenet.com/sudden_cardiac_death/article.htm http://www.cvphysiology.com/Arrhythmias/A008.htm |
